Our FNP Curriculum Review book is a great addition to help you master the FNP material, and will help you excel on your national certification exam!
With over 800 unique practice questions and over 600 pages of content, this culminating work combines material from Barkley’s Curriculum Review for Adult-Gerontology Primary Care Nurse Practitioners and Barkley’s Curriculum Review for Pediatric Nurse Practitioners to provide a comprehensive overview of adult and pediatric content.
Includes
600+ Pages
Shipped in
1-2 business days
$149.95
$129.95
Ace your school exams and boards with our FNP practice book!
Covering assessment, labs/diagnostics, management/treatment, pharmacology, and professional practice
For quick reference when treating patients
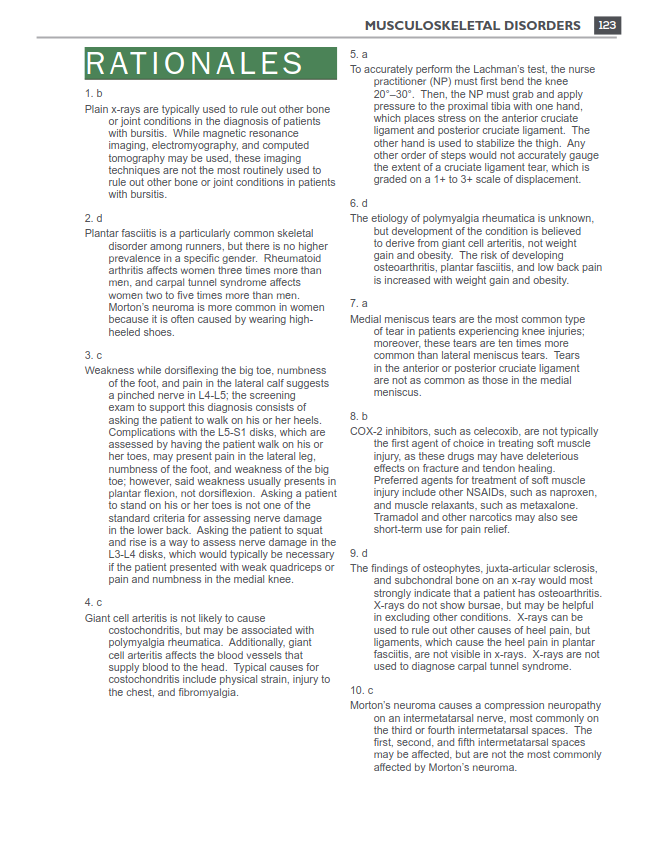
Allow students to identify areas of strength, and extensive discussions provide a comprehensive overview to supplement areas of weakness
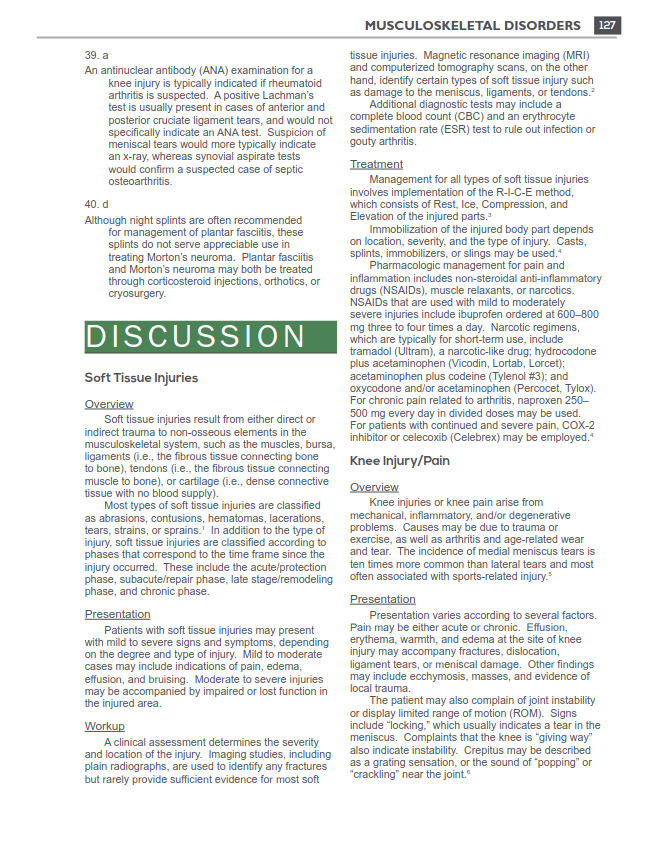
Questions, rationales, and discussion along with tables and figures